What is a Lower Limb Discrepancy?
The term “lower limb discrepancy” means the finding of a difference in length between the two limbs and is a really frequent occurrence.
A discrepancy in the lower limb is often highlighted during a pediatric or orthopedic control visit. This difference in length may range from small asymptomatic situations, which require no treatment, to a very severe amount, requiring demanding reconstructive surgeries.
One aspect of managing of the lower limb discrepancies in the pediatric age, is to consider them as dynamic problems, which can change during the growth.
The human body is characterized by a variable symmetry, which is more properly called “physiological asymmetry”.
A moderate and asymptomatic difference in the length of the lower limbs is very common. A meta-analysis study, published by Knutson in 2005, showed that only 10% of the adult population examined had the same length of the lower limbs, compared to a discrepancy equal to or less than 1 cm found in almost 90% of the population.
We can find many causes of lower limb discrepancies in children, generally divided into three categories:
- congenital
- developmental
- acquired.
However, it must be specified that in 95% of the cases the causes remain unknown.
CONGENITAL
The difference in length is already evident at birth. Among the most common congenital causes are femoral hypoplasia (see LINK), fibula hemimelia (see LINK), tibial hemimelia, idiopathic hemihypertrophy.

DEVELOPMENTAL
In this group the length discrepancy becomes evident during the growth. It is mostly due to an underlying congenital or genetic pathology, for example in case of a congenital clubfoot (see LINK), multiple enchondromatosis, hereditary multiple exostoses (see LINK), neurofibromatosis, congenital pseudartrosis of the tibia, vascular abnormalities (e.g. Klippel-Trénaunay…).

ACQUIRED
To this group belong changes that arise as a result of traumatic events (long bone and physeal fractures), infections, bone cancer, radiation therapy, rheumatic diseases, or as a consequence of orthopedic conditions such as Perthes disease (see LINK), Blount’s disease (see LINK).

Is the limb too long or too short?
Another important distinction is to understand if the problem of the length discrepancy comes from the longest limb or the shortest limb:
- Too long may be a limb that grows more than it should, for example as a result of an overgrowth: hemihypertrophy, macrosomy, ILO, etc, or a vascular pathology affecting the limb (s. Klippel-Trenaunay, Parks-Weber, etc.) or following a fracture of the femur that stimulates the growth of the limb (post-traumatic overgrowth).
- Too short may be a limb that grows less, because of congenital (hypoplasia, etc.), developmental (exostosis, etc.) or acquired (growth cartilage injury, etc.) problems.
It is not always possible to establish this distinction, and, especially in case of small lower limb discrepancies, it is impossible or not useful. Instead, it becomes really important for significant discrepancies, especially when a surgical correction is needed.
In these cases, one of the rules that should guide the therapeutic choice is, where possible, to treat the limb that has the problem: in other words, shortening the longer limb or lengthening the shorter limb.
What does the lower limb discrepancy entail?
During the past, it has been supposed the association between a lower limb discrepancy and the development of scoliosis, lumbar pain, pain at the lower limbs, osteoarthritis (due to over-stress, especially to the longer limb), and falls.
A meta-analysis study published by Gordon in 2019, seems to confirm the evidence that length discrepancies bigger than 2 cm would be associated with a higher incidence of problems (especially osteoarthritis, but also lumbar pain). The clinical consequences of lower limb discrepancies inferior to 2 cm are less clear.
In the presence of a limb discrepancy (especially when it is more than 3% of the total length), the body applies compensation processes, as: bending and / or circumduction of the longest limb, or equinus (walking on the tip of the foot) of the shorter limb. For differences of length greater than 5.5% it becomes more and more difficult for the body to compensate the asymmetry.
How to assess the limb discrepancy?
The control of the growing subject must include the assessment of a possible length discrepancy of the lower limbs at the time of periodic health balances. Without pain or discomfort, children can hide a leg length difference very well. Thus, a proper clinical evaluation is very important.
The difference in length can be:
- STRUCTURAL: as a consequence of a real discrepancy between the two limbs
- FUNCTIONAL or POSTURAL: the difference is not due to a real shortening of a limb, but is illusory, as a result of an asymmetric position of a lower limb (for example in case of a contracture in adduction of a hip, or pelvic obliquity).
The clinical examination should be performed with the patient lying supine and in standing position.
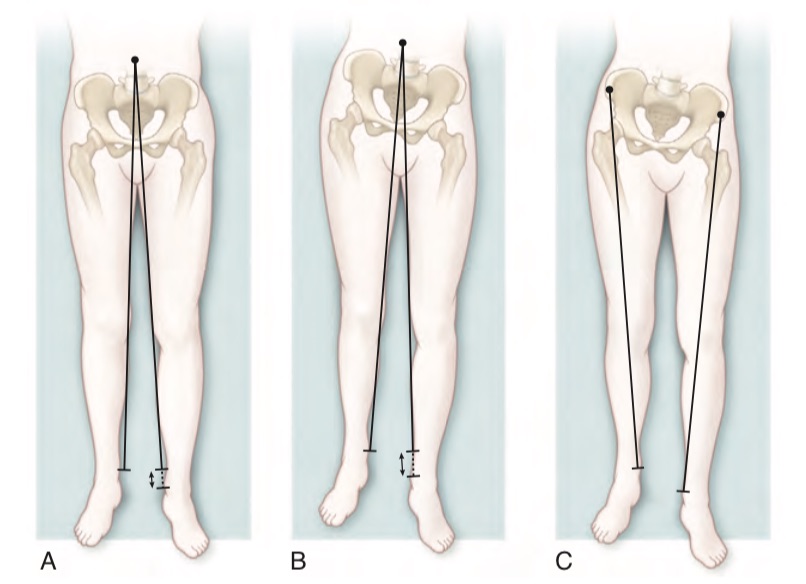
With the patient in supine position (with the pelvis aligned, and the legs extended and parallel), a lower limb discrepancy can be roughly identified comparing the level of the malleoli. The measurement of the distance between the anterior-superior iliac spine and the malleolus on both sides is theoretically more appropriate, but is often burdened with errors, and it has a low reproducibility.
It is also possible to compare the length of the two limbs by dividing the analysis into segments:
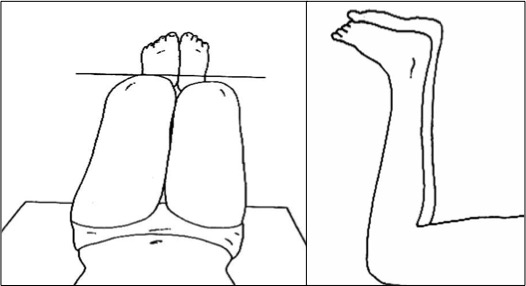
- Pelvic-femur segment: with the hips flexed, the level of the knees is observed (so-called “Galeazzi’s sign”)
- Leg-foot segment: with the patient in prone position, the level of the malleoli and feet is observed
This distinction makes it possible to understand if the problem is located mainly in the proximal (for example, following a fracture of the femur) or distal segment (for example, a fibular hemimelia).
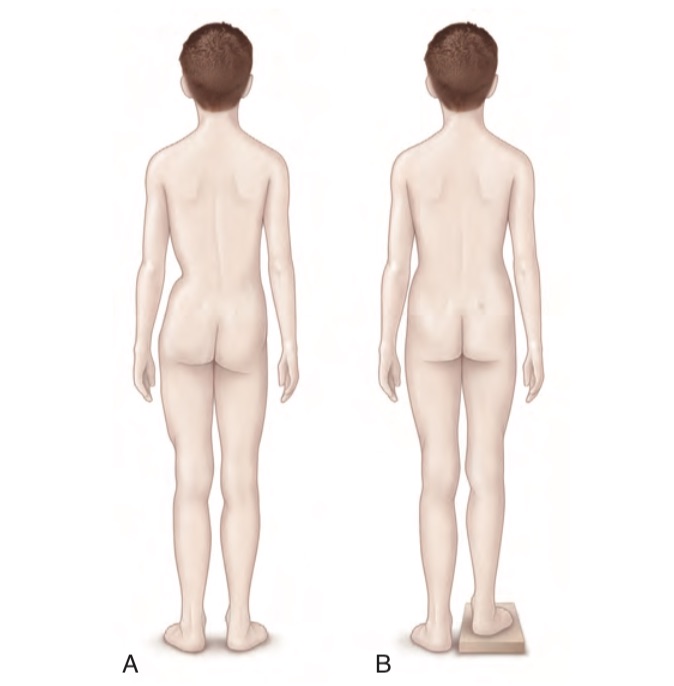
In standing position, with the feet well-placed on the ground and the knees fully extended, the examiner, placed behind the patient, can observe a different height of the iliac crests, of the sacral dimples and of the popliteal plications.
When a different height of the iliac crests is observed, positioning of a wedge under the foot of the shorter limb (until it is matched) allows a quick measurement of the discrepancy.
Assieme alla valutazione dell’eterometria, è sempre importante controllare la motilità articolare dei vari distretti, la posizione degli arti a riposo, eventuali deformità angolari, anomalie cutanee o dei tessuti molli, ed in fine lo stato neurologico (forza muscolare e riflessi).
Radiographic examination, when and how should it be done?
The radiographic examination is very useful to evaluation the limb discrepancy. It should be performed after a specialist indication, and it should be executed only in case of a significant difference (exceeding 1/1.5 cm).
The difference in length is confirmed with a panoramic radiography (extending from the pelvis to the feet) in standing position.
For proper examination, the patient should be positioned:
- With the limbs fully extended (one knee should not remain flexed)
- Without stressing any varum or valgum (if valgum is present, the knees must be held so that they barely touch, and in case of varum, so that the feet touch)
- The patellas should look straight forward
- The femoral and ankle must be on the same X-ray
- The iliac crest and the triradiate cartilage must be included
In the case of lower limb discrepancies greater than 2-3 cm, it is important that the examination is carried out with a wedge under the foot of the shorter limb. The amount of the lift should be indicated by the specialist to the radiologist, and usually corresponds to the estimated discrepancy. Performing of the x-ray without the wedge exposes to the risk of wrong measurement of the difference in length (the patient normally flexes the knee of the longer limb, falsifying the X-ray image and the measure).

BIBLIOGRAPHY
- Tachdjian’s Pediatric Orthopaedics – 5th Ed – Elsevier (2014_Vol 2_pag 884-891)
- Knutson GA. Anatomic and functional leg-length inequality: a review and recommendation for clinical decision-making. Part I, anatomic leg-length inequality: prevalence, magnitude, effects and clinical significance. Chir Ost 2005
- Tallroth K. Preoperative leg-length inequality and hip osteoarthrosis: a radiographic study of 100 consecutive arthroplasty patients. Skeletal Radiol. 2005.
- Tallroth K. Is a long leg a risk for hip or knee osteoarthritis? Acta Orthop. 2017.
- Gordon JE. Leg Length Discrepancy. The Natural History (And What Do We Really Know). JPO 2019
Go to Epiphysiodesis surgery to correct the lower limb discrepancies
Go back to the Center for Lower Limb Deformities


