
Genu Varum: physiological, idiopathic and secondary.
Genu Varum (or Bow legs) is an alteration of the axis of the lower limbs that appear like round brackets (bow legs).
The distance between the two knees is increased, as opposed to the valgus knee, which has an X-shaped appearance.
The varus deformity can affect only one limb or both.
From a technical point of view, the mechanical axis of the lower limb (the line that connects the centre of the hip with the centre of the ankle), in normal situations passes through the centre of the knee thus distributing the load symmetrically.
In the case of genuflects varum, the mechanical axis falls more inside; in this way, the joint undergoes (both in an upright position and during walking) a non-physiological stress, both on the articular cartilage and ligaments.
Physiological genu varum.
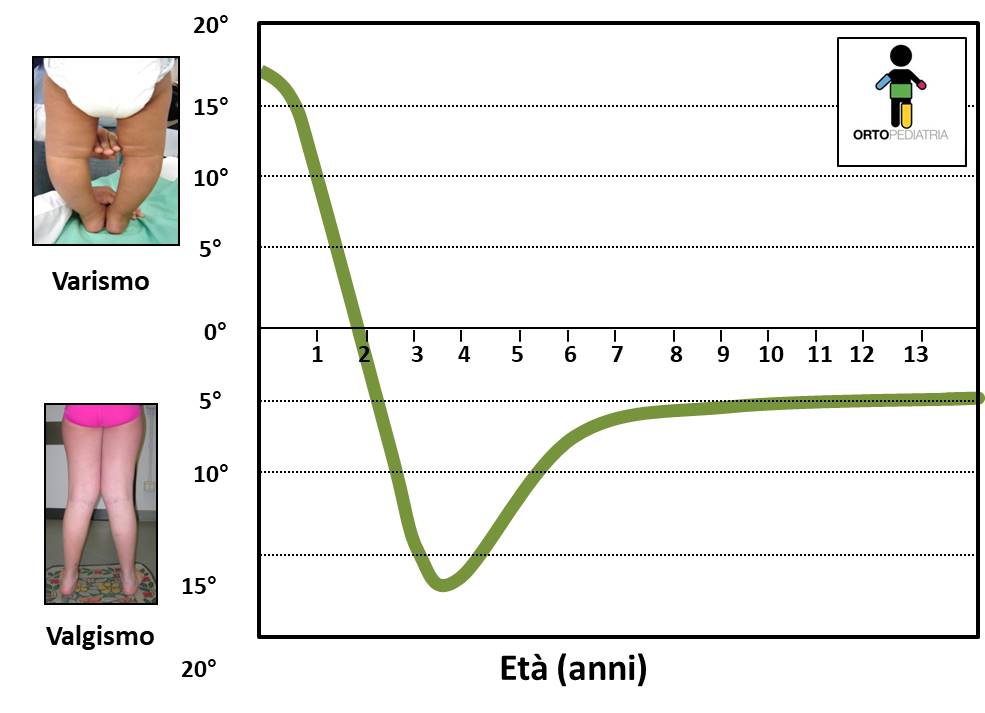
The physiological development of the axis of lower limbs in children has a typical course.
At the beginning of walking, up to about 18 months of age, most children show a (more or less marked) varus axis of their knee, that can be considered physiological.
The axis tends spontaneously to evolve towards a second phase of valgus (X-shaped knees). Also this second phase is usually transient: the deviation can be more or less accentuated, reaches the peak of valgus around 3.5-4 years, then the axis returns spontaneously towards the neutral axis, reaching at the age of 7-8 years the axis typical of adulthood (physiological valgus).
Idiopathic and secondary genu varum.
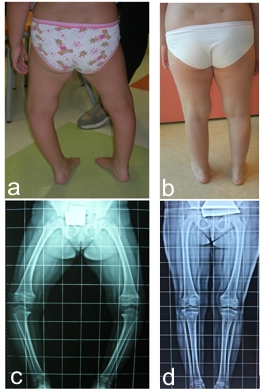
This phase of physiological varus knee is often a cause of concern for families, and doctors must be able to distinguish the physiological cases for which follow-up is sufficient without treatment, from pathological cases that require early treatment.

In older children, varus axis should no longer be present and the physician should be able to distinguish between an idiopathic genu varum (that is constitutional, often on a family basis and without underlying pathologies) and a secondary genu varum, where there is an underlying pathology that causes the deviation.
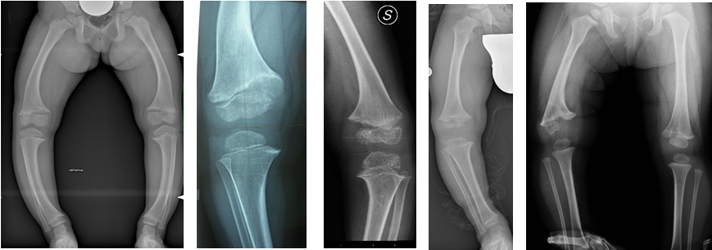
Among the possible causes of secondary genu varum, we can find different conditions, for example: deficiency rickets, vitamin D-resistant rickets, rickets from renal pathology, skeletal dysplasia (achondroplasia, hypochondroplasia, pseudochondroplasia, etc.), multiple hereditary exostosis, osteogenesis imperfecta, consequences of infection or trauma on the growth cartilage, as well as Blount’s disease.
Treatment.
In the idiopathic varus knee, treatment can range from simple observation, to adequate hygiene rules (weight control, etc.), to the possible integration of vitamins under the supervision of the paediatrician, to the use of orthoses/orthopaedic footwear (now limited to very few and selected cases), up to surgery.
Varus knee surgery can range from less invasive interventions, such as asymmetrical epiphysiodesis with “8-plates” (guided growth), in the case of children with active growth cartilage, to more invasive interventions, such as corrective osteotomies.
In secondary knee varus, in addition to the axis defect, the underlying pathology must be taken into account (which in some cases can and should be treated, for example in deficiency rickets), which is often associated with greater difficulty in treatment and a tendency to relapse.
Temporary asymmetrical epiphysiodesis (guided growth)
The term epiphysiodesis means a procedure on the growth plate that aims to stop (or slow) the activity of a part of (or all) the growth cartilage.
Growth cartilages (also called physes) are the typical structures of children’s bones that allow the various bone segments to grow in length. They can be represented as discs of cartilage at both ends of a long bone, in which the cartilage cells reproduce longitudinally and progressively ossify, thus increasing the length of the segment.
Such cartilages are active throughout the growth of the child and end their activity with skeletal maturity, when the cartilage closes and is completely replaced by bone.

In the case of asymmetrical epiphysiodesis: the physis is slowed (by the procedure) only on one side, while the remaining part of cartilage continues to grow normally. This determines a deviation of the growth: if the internal part is slowed, only external growth will continue, and vice versa.
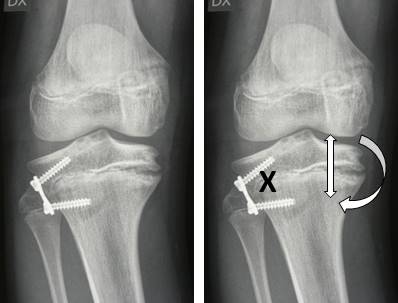
The most commonly used tool for epiphysiodesis is the so-called 8-plate for guided growth (the plate has a shape of 8).
These plates, in the varus knee, are placed in the lateral part of the growth cartilage of the knee (tibia or femur) and fixed to the bone by two screws. The surgical incision is limited to 3/4 cm. No immobilization is required, gradual mobilization of the knee starts early and progressive load is allowed.
If correctly applied, the plates gradually determine the correction of the axis, with a speed proportional to the growth of the operated limb.
It is a procedure capable of significantly changing the growth of the limbs, which can give remarkable results in the face of low invasiveness. Clearly in patients at the end of growth, there is no possibility to perform such an intervention, and the only alternative to varus knee correction remains osteotomy. This is why it is essential that patients are promptly referred to the paediatric orthopaedic surgeon, in time to make the appropriate assessments.
This epiphysiodesis is a temporary procedure: once the desired goal (the correct axis) is reached, the plates can be removed in order to restart the growth of cartilage. It is therefore a theoretically reversible procedure.
However, there are two risks to consider:
• the risk of lesions of the growth cartilage produced at the time of surgery and by the plate itself: once the plate have been removed, if there is still growth of the cartilage on the opposite side, the knee may continue to deviate in the direction of correction, leading to hypercorrection (valgus knee)
• the “rebound” effect: once the plates have been removed, the area of cartilage that has been slowed begins to grow excessively, leading to a recurrence of the varus knee
For this reason, it is necessary to perform the procedures with the correct technique and it is often preferable (when possible) to perform the intervention near the end of the growth, so as to obtain the correction of the axis and no longer have further growth that is likely to cause hypercorrection or recurrence.
In cases where the varus knee is very marked and the patient is still small, as in cases of skeletal dysplasia, it is preferable to intervene early, remove the plates once the axis is corrected, and verify the successive evolution. It will be possible to repeat the procedure if the deformity recurs.
The basis of all this is a correct pre-operative assessment.
Clinical and radiographic aspects must be taken into account before treatment with epiphysiodesis. Radiographic evaluations are essential to avoid unnecessary corrections. The surgical indication should be limited to cases with significant alteration of mechanical axis.
Another fundamental aspect is to calculate as precisely as possible the timing of the procedure, evaluating for example the speed of growth in height, pubertal development, bone age.
The last fundamental aspect is the postoperative follow-up, initially to verify that the recovery of knee function is regular, then to verify the effect of the intervention.
Radiographs are performed periodically, to check the evolution of the mechanical axis.
Overall, epiphysiodesis is a non-invasive procedure for the patient, with excellent results.
Take a look at:
Back to Pediatric Orthopedics


